Eye Conditions
When looking at your eye health during a routine eye examination, we are always on the lookout for whatever is out of place. The sorts of diseases that concern us most, however, are the ones that most often cause permanent vision loss. Unfortunately, many eye diseases can be progressing without symptoms until at a late stage when very little can be done. The conditions most famous for this include: Diabetic Retinopathy, Macular Degeneration, and Glaucoma. And discussing these three may give you a feeling for the kind of things we look for in a routine examination at our office, and hopefully instill some fear and respect for eye diseases. There are many, many more eye diseases that could be discussed here, and we may add more articles to our website’s library in the future. But these three diseases are the ones that break our heart most often as examiners because even though they can be slowed or stopped when diagnosed, we still see patients neglect examination and treatment and lose their vision from them.
Diabetes
The number of diabetics has nearly tripled in this country since 1980. According to the American Diabetes Association (www.diabetes.org), 25.8 million children and adults in the U.S. have diabetes - this is 8.3% of the population! Of these, 25-30% are unaware that they have it, but even more alarming is that three times as many people, about 79 million, are pre-diabetic. According to the NEI (www.nei.nih.gov), approximately 10.2 million Americans over age 40 are diagnosed diabetics. The NEI also estimates that 40% of diabetics over age 40 have some degree of diabetic retinopathy, with one of every 12 diabetics in this age group having progressed to the severe, vision-threatening stage. The retina, the light-sensitive part of the eye that sends the vision signals to the brain, is the part that we examine most closely when you have diabetes.
Diabetic Retinopathy has become the most common cause of new blindness cases in the U.S. for people between 20 and 74 years old. (Over 74 and it becomes Macular Degeneration… read below.) The main reason for this is a loss of circulation. A glucose (sugar) level that is too high inside the body’s cells is toxic to them, eventually causing them to die. If circulation is poor enough, the cells will rot (gangrene). (This is also one of the reasons for diabetes being 60% of all amputations - about 82,000 annually!) Most cells of the body don’t allow sugar to enter inside unless insulin is present. The exceptions to this are the cells of the retina, kidneys, and nervous system, which simply soak it in. This is why these kinds of cells are far more prone to damage from high glucose levels.
The main kinds of diabetes are type 1, (about 5% of cases), and type 2, (by far the majority). Type 1 is where the body does not make insulin because the pancreas has been damaged. These people must receive it from outside (injections or pump) or death will occur. Type 2 diabetes happens when the cells of the body no longer respond to insulin, and don’t take in sugar as they should. This is called “insulin resistance.” Because of this resistance, the pancreas, which makes the insulin, eventually fails from having had to produce high levels of insulin, and insulin then has to be added from outside as in type 1 diabetes. The medications used to help type 2 work by helping the cells react to insulin. Technically it is not known why type 2 happens, but it has been strongly associated with obesity, genetic risk factors, and inactivity.
The main mechanism of cell damage comes from cell chemistry. A glucose level over 150 inside a cell is poisonous to it, pushing the cell to use an unhealthy alternate chemical pathway called the polyol pathway to burn the excess glucose that has gotten inside. This produces compounds that cause cell damage and eventually death, mostly by making it almost impossible to regulate water content. Blurriness and variable vision come from this, among other chemical situations Diabetes creates. If enough cell damage and death occurs, new blood vessel networks form (neovascular proliferation). These networks are weak and burst, putting raw blood into the retina. This causes scarring, the death of retina cells, and eventually blindness. Proliferation is the big divide in diabetic disease course: once this is crossed, prognosis is much worse.
Glucose levels are generally considered within normal if they remain between 80 and 130. Maintaining blood glucose levels within this range, and keeping them at even levels preserves tissue health. The numbers used to describe the rate at which calories are broken down and delivered to the cells of the body are the ‘Glycemic Index’ and ‘Glycemic Load’. Choosing a diet of low-load, slow-burning foods helps control the sugar levels more easily, and is a more effective method of preventing the progression of disease than the use of medications to compensate for poor dietary choices. Antioxidant supplements also help to protect the retina from damage due to diabetes, macular degeneration, and a host of other things.
Diabetics should have a dilated retinal examination at least every 12 months if there is no evidence of retina damage, every 6 months if there are early signs, and every 3 months or sooner if significant diabetic damage is happening. Prevention is the best medicine: the best treatment for diabetic retinopathy is careful management of blood sugar levels, but there are excellent new treatments which improve vision and prolong sight in those with diabetic retinopathy. In order to reach treatment, however, the condition must be diagnosed first! Schedule an appointment if you are being treated for blood sugar problems! And when you come in, bring the contact information for the physician who is managing your diabetes so that we can send them a brief report of your diabetic eye exam.
Macular Degeneration
The light-sensitive tissue on the back of our eyes that sends messages to our brains about what we see is called the retina. It is a thin sheet of Central Nervous System tissue which contains two kinds of light-receiving cells: cones, which are specialized to see color and detail; and rods, which have a quick response to motion. Being part of the Central Nervous System, it doesn’t grow back if damaged (just like a spinal-cord injury.) The macula is the area in the center of the retina specialized for seeing small details. It is 1.5mm in diameter, which makes up the central 13 degrees of the visual field. The central 3 degrees of the macula is called the fovea, and the only place you see '20/20'. The macula sees small detail because it has the highest concentration of cones and other specializations. The rest of the retina has fewer and fewer cones as you move toward the periphery, and has a quick response to movement—an amazing design.
The full name for the macula is the macula lutea, meaning ‘yellow spot’ in Latin. This yellowish color is from several similar pigments, the most important of which are Lutein and Zeaxanthin. These pigments can be found in food, generally from things that are darkly pigmented such as berries and dark green vegetables. These sorts of compounds are from a family of nutrients called antioxidants, the most common members of which are vitamins C, E, and A. Along with many other helpful effects, these can help prevent Macular Degeneration according to large national studies such as the AREDS studies, which studied the use of supplements. According to research, most nutrients are taken up together and aren’t absorbed nearly as well individually. This makes sense: the body is designed to absorb nutrients out of food, where all things are mixed together. The most easily absorbed forms of vitamins are in food, but in order to get the amount you need requires a lot of dietary dedication! A balanced multivitamin supplement is the most certain way to get the vitamins you need, preferably one where the most absorbable forms of the vitamins are used. (The best delivery forms are those that dissolve fully, such as capsules or liquids rather than compressed tablets.)
There are two main forms of macular degeneration, depending the layers of the retina affected. These are referred to as the non-exudative (“dry”) form, which is the most common and is less catastrophic; and the exudative (“wet”) kind, which more commonly has a genetic part and tends to be more severe and sight-threatening. Sometimes severe cases of the non-exudative form will spread to more layers of the retina and progress to the more destructive exudative kind. There are more treatment options available for the destructive ‘wet’ form than the ‘dry’ form. In the exudative form, as in diabetic retinopathy, neovascular networks can form, which cause scarring as they leak and break. The most effective innovation in recent years to treat neovascularization is the use of drugs that suppress the action of a family of chemicals called Vascular Endothelial Growth Factor (VEGF). These are chemical messengers that the body uses to stimulate new blood vessel growth. These powerful anti-VEGF medicines are put directly into the eye, and often improve vision vastly. All this can be done if only people would come in for exams so they can be diagnosed!
Glaucoma
This is a serious eye disease where the pressure in the eye is high enough to cause damage to the signal-carrying nerve fibers of the eye. This damage happens to the weakest part of the eye’s structure, the place in the back where all the nerve fibers go out to connect to the brain. In other words, the high pressure strangulates the eye’s wiring, and the resulting damage is called glaucoma. It is estimated that up to one percent of the US population has this, and only one half are diagnosed - between two and three million people.
The eye is kept properly inflated by the fluid-filled front chamber of the eye. A clear fluid called the aqueous is gradually produced behind the iris, and flows through the pupil to gradually drain in the corner between the cornea and the iris. Production and drainage of fluid should result in the eye being inflated to a normal range of pressure between 8 and 21 units. If this fluid is over-produced or else doesn’t drain well enough, excessive pressure is created which does the damage. There are, then, different kinds of glaucoma, named for whether the fluid is overproduced or doesn’t drain. By far the most common kind is the over-production kind, called ‘open angle’ glaucoma because the drainage structure is normal, but is overwhelmed. This kind is, unhappily, the kind with no symptoms from the patient’s perspective, and is the most subtle to detect from the physician’s perspective. The key to preventing blindness from this is diagnosis in the first place! Once damage occurs to the retina it is permanent. Most often, the treatment is simply taking a drop once or twice a day to keep the pressure down, and having brief checkups about once every three months.
Diagnosis is made easier when risk factors are taken into account, which include age, family history (especially sister or brother), extended genetic history (race), diabetes, and high myopia. National studies show, for example, that African-Americans have an incidence of glaucoma five times higher than Caucasians, and blindness happens fifteen times more often in those between the ages of 45 and 64 than in Caucasians of the same age. Put simply, it happens more often, and when it does it is much more aggressive. Hispanic patients over 60 also have cases as severe if not more so. The damage happens more slowly in the open-angle kind, however, than in cases where the other part of the eye’s fluid exchange mechanism is abnormal, what is called narrow-angle glaucoma.
Pressures spike very rapidly in an eye when the drainage structure is closing off, and very severe pain and nausea normally occur, along with blurry vision. Patients with this kind of glaucoma are at greatest risk of rapid damage since their pressures can rise to very high levels (50 or more!): angle closure is a true ocular emergency. Patients usually report having had painful episodes beginning in their teenage years. These episodes most often happen to people whose eyes naturally have a narrow space between their cornea and iris (“narrow angles”). These episodes happen like this: when the fluid cannot get out fast enough, the peripheral iris billows forward toward the cornea to the point of sticking to it, closing off the drainage angle completely. Once a part of the iris does this, the pressure rises further, causing more of it to billow forward until the entire angle is closed off. Once patients have had this happen, surgery is done to prevent this complete-closure situation where a small opening is made in the peripheral iris to allow fluid to escape in the event that pressure begins to rise (usually done on the top, under the upper lid). This is very helpful, but medications are normally used in addition to this to help prevent the pressures from getting close enough to cause an attack. It is also possible that an eye both over-produces and has a faulty drainage mechanism— both kinds at the same time— but this happens very rarely.
Other ways that glaucoma occurs are when cells from the front chamber of the eye clog up the drainage angle. These conditions include Pseudo-Exfoliation Syndrome (the front surface of the crystalline lens peels), Pigmentary Dispersion Syndrome (the pigment on the back surface of the iris sheds), and bleeding (hyphema). When people receive a sharp poke in the eye for example, bleeding can occur in the front chamber of the eye, and the blood can clog the drainage angle causing a pressure spike that can cause a permanent loss of sight. This is a very dangerous condition that a physician looks for when a patient comes in having had a sharp blow to the eye. Just as in angle closure glaucoma, the pressures can spike violently, and heroic measures have to be taken quickly to preserve sight.
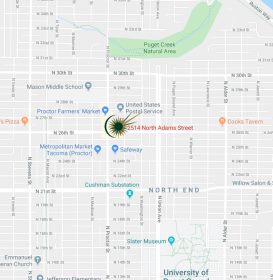
All routine comprehensive examinations check for these three things and much more; when we examine your eyes, we are looking for anything that is out of place. Early diagnosis decreases the chances for permanent vision loss, so call us to make an appointment today at (253) 759-5679.
Though every effort has been made to be accurate, all articles contained within this website are for strictly informational purposes, and not to be used as a sole source for healthcare training and instruction. Neither does Family Vision Center of Tacoma, P.S., assume responsibility for actions undertaken by someone using information presented on this website to make healthcare decisions.
Glowing Reviews
Everyone was great and served me very attentively. Thank you very much for listening to my concerns and helping me all the way from a thorough exam to picking a pair of glasses that work perfectly for me! What a relie
Lorrie, Tacoma
We are thrilled to have finally discovered our neighborhood eye doctor! We love it and had a great experience!
Ron, Tacoma
Thank you for a comfortable eye exam experience! Friendly staff, professional office environment - I am so glad I found you guys.
Linda, Roy, WA
Just wanted to make it official that you are the best! You all are so professional, knowledgeable and welcoming. I appreciate coming to a place that I can trust always knowing I’m in good hands with people
Claire, Tacoma
I was very pleased and felt like a person not a numbered patient. Thank you!
Brenda, Tacoma